Ear Infection Was Better and Started Hurting Again
Chronic ear infection is fluid, swelling, or an infection behind the eardrum that does not go abroad or keeps coming back. It causes long-term or permanent damage to the ear. It often involves a hole in the eardrum that does not heal.
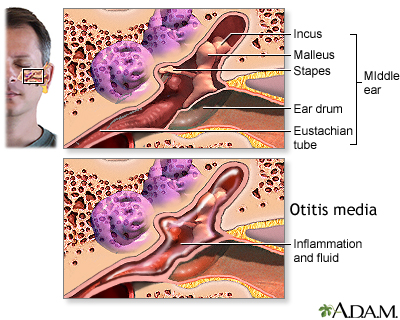
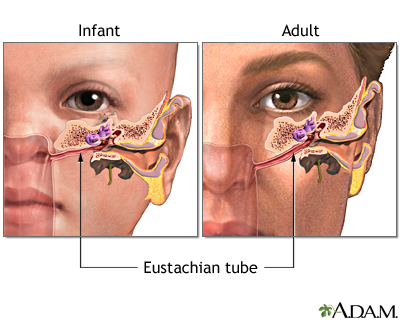
The eustachian tube runs from the middle of each ear to the dorsum of the pharynx. This tube drains fluid made in the eye ear. If the eustachian tube becomes blocked, fluid can build up. When this happens, infection tin occur. A chronic ear infection develops when fluid or an infection backside the eardrum does non go away.
A chronic ear infection may be caused past:
- An astute ear infection that does non completely go away
- Repeated ear infections
"Suppurative chronic otitis" is a term used to depict an eardrum that keeps rupturing, draining, or swelling in the middle ear or mastoid area and does non go away.
Ear infections are more common in children considering their eustachian tubes are shorter, narrower, and more than horizontal than in adults. Chronic ear infections are much less mutual than astute ear infections.
Symptoms of a chronic ear infection may be less severe than symptoms of an acute infection. The trouble may go unnoticed and untreated for a long time.
Symptoms may include:
- Ear pain or discomfort that is usually balmy and feels similar force per unit area in the ear
- Fever, usually low-grade
- Fussiness in infants
- Pus-like drainage from the ear
- Hearing loss
Symptoms may go along or come and go. They may occur in ane or both ears.
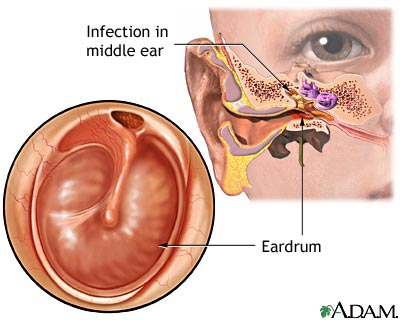
Your wellness care provider will look in the ears using an otoscope. The exam may reveal:
- Dullness, redness in the middle ear
- Air bubbles in the center ear
- Thick fluid in the middle ear
- Eardrum that sticks to the bones in the center ear
- Draining fluid from the eardrum
- A hole (perforation) in the eardrum
- An eardrum that bulges out or pulls back inward (collapses)
Tests may include:
- Cultures of the fluid that may testify a bacterial infection.
- A CT scan of the head or mastoids may prove that the infection has spread beyond the middle ear.
- Hearing tests may be needed.
The provider may prescribe antibiotics if the infection is caused past bacteria. These medicines may need to be taken for a long time. They tin be given by mouth or into a vein (intravenously).
If there is a hole in the eardrum, antibody ear drops are used. The provider may recommend using a mild acidic solution (such equally vinegar and h2o) for a difficult-to-treat infected ear that has a pigsty (perforation). A surgeon may need to clean out (debride) tissue that has gathered inside the ear.
Other surgeries that may be needed include:
- Surgery to clean the infection out of the mastoid bone (mastoidectomy)
- Surgery to repair or supersede the small bones in the middle ear
- Repair of the eardrum
- Ear tube surgery
Chronic ear infections often reply to treatment. Notwithstanding, your child may demand to keep taking medicines for several months.
Chronic ear infections are not life threatening. However, they can exist uncomfortable and may result in hearing loss and other serious complications.
A chronic ear infection may cause permanent changes to the ear and nearby bones, including:
- Infection of the mastoid bone behind the ear (mastoiditis)
- Ongoing drainage from a hole in the eardrum that does not heal, or later on ear tubes are inserted
- Cyst in the centre ear (cholesteatoma)
- Hardening of the tissue in the middle ear (tympanosclerosis)
- Harm to, or wearing abroad of the basic of the middle ear, which help with hearing
- Paralysis of the face
- Inflammation around the brain (epidural abscess) or in the brain
- Damage to the office of the ear that helps with rest
Hearing loss from damage to the middle ear may slow language and voice communication evolution. This is more likely if both ears are afflicted.
Permanent hearing loss is rare, but the run a risk increases with the number and length of infections.
Call your provider if:
- Y'all or your child has signs of a chronic ear infection
- An ear infection does non reply to treatment
- New symptoms develop during or subsequently treatment
Getting prompt treatment for an acute ear infection may reduce the risk of developing a chronic ear infection. Have a follow-up exam with your provider later on an ear infection has been treated to make certain that it is completely cured.
Eye ear infection - chronic; Otitis media - chronic; Chronic otitis media; Chronic ear infection
Chole RA, Sharon JD. Chronic otitis media, mastoiditis, and petrositis. In: Flint Pow, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 140.
Ironside JW, Smith C. Central and peripheral nervous systems. In: Cantankerous SS, ed. Underwood's Pathology. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 26.
Kerschner JE, Preciado D. Otitis media. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 658.
Pelton SI. Otitis externa, otitis media, and mastoiditis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Do of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 61.
Rosenfeld RM, Schwartz SR, Pynnonen MA, et al. Clinical practice guideline: Tympanostomy tubes in children. Otolaryngol Head Neck Surg. 2013;149(1 Suppl):S1-S35. PMID: 23818543 pubmed.ncbi.nlm.nih.gov/23818543/.
Rosenfeld RM, Shin JJ, Schwartz SR, et al. Clinical practise guideline: otitis media with effusion (update). Otolaryngol Head Cervix Surg. 2016;154(ane Suppl):S1-S41. PMID: 26832942 pubmed.ncbi.nlm.nih.gov/26832942/.
Steele DW, Adam GP, Di Chiliad, Halladay CH, Balk EM, Trikalinos TA. Effectiveness of tympanostomy tubes for otitis media: a meta-analysis. Pediatrics. 2017;139(6):e20170125. doi:10.1542/peds.2017-0125. PMID: 28562283 pubmed.ncbi.nlm.nih.gov/28562283/.
Updated by: Neil M. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Internal review and update on 06/03/2021 by David Zieve, Doctor, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Source: https://medlineplus.gov/ency/article/000619.htm
0 Response to "Ear Infection Was Better and Started Hurting Again"
Post a Comment